Health Professional COVID-19 and Cancer Hub

Cancer Research UK supports GPs to deliver best practice
If you have any questions or feedback on the about this information please get in touch.
Key resources to support health professionals
COVID-19 has had far-reaching impact, with significant alterations in health services across the UK, including screening, cancer diagnostics, pathways, and treatment, as well as changes in public confidence and behaviour.
At Cancer Research UK, we have been working to keep on top of the latest intelligence, data, research and guidance that both allows us to understand what the impact of COVID-19 continues to be on cancer services, and how we might best mitigate it.
On this page you can find links to COVID-19 related information and resources that have been developed for health professionals. Each resource is being kept under review and will be updated with new information as and when required.
If you are looking for patient facing information, please see our COVID-19 and Patient Cancer Hub.
COVID-19 and cancer key stats - Updated October 2022

COVID-19’s effect on cancer patients is a key concern to the cancer community with delayed or decreased diagnosis, tests and treatment. To understand this variable and rapidly changing landscape the Cancer Intelligence team are regularly monitoring published data around the impact of the pandemic across the cancer pathway. We have prepared some key insights which reports latest data across the UK (and where possible for the devolved nations) on screening, urgent suspected referrals, diagnostic tests and treatment.
Cancer Intelligence Team, Cancer Research UK.
Performance measures across the cancer pathway: Key Stats
Updated October 2022.
COVID-19 has had a significant impact on primary care – patient presentation levels decreased, and CRUK estimates Around 430,000 fewer people than normal in the UK were on an urgent suspected cancer referral during March 2020-February 2021 compared with the same time the previous year.
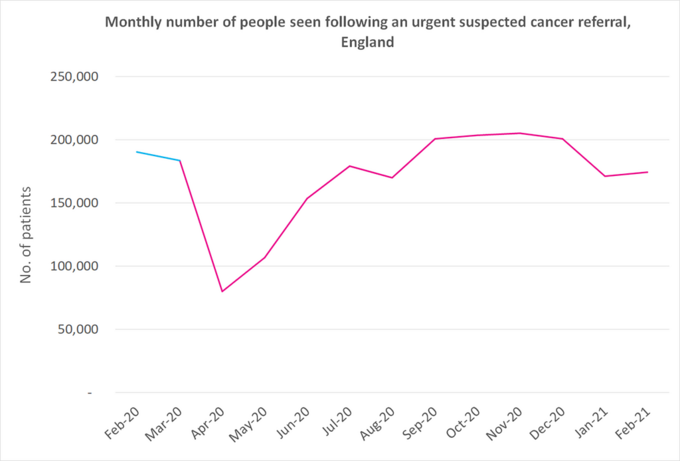
Overall, the number of urgent suspected cancer referrals seen in secondary care dropped to the lowest point in April 2020 with around a 60% decrease compared to April 2019 (according to data from England and Wales). Since then, the numbers have been steadily improving, but according to e-Referrals Service data in England, In September numbers were, for the first time since March, around the same level as the previous year. Numbers stayed approximately similar to the previous year’s levels through to December too, with 2% more referrals, or around 3,700 more patients (around 200,900 in December 2020 compared to around 197,200 in December 2019). The graph below shows the impact on the weekly number of urgent suspected cancer referrals in England between February 2020 and February 2021. Referrals for some cancer types such as lung cancer have been more impacted than others and are further behind recovering.
Monthly numbers of urgent (2ww) suspected cancer referrals, England (CWT data)
This is mirrored by a decrease in diagnostic testing – in England, over March 2020-February 2021 there was a 24% reduction in the number of key radiology and endoscopy tests undertaken (around 4.6 million fewer of these were undertaken compared to the same time in the previous year).
Lung cancer can be challenging to diagnose even under normal circumstances; therefore, it is more important than ever to be alert to the risk of suspected lung cancer in your patients, with the added possibility of symptoms now being disguised by potential COVID-19 symptoms.
The lung cancer pathway continues to be particularly affected by the COVID-19 pandemic and has been slow to recover.
Around 25,900 fewer people were referred via urgent suspected lung cancer referrals in England during March 2020 to August 2021 compared to the same months in 2019, a reduction of 26%. However, the number of patients starting treatment in England in August 2021 was similar to what we would have expected if the pandemic had not happened, therefore people were possibly coming through other routes.
While the equivalent data isn’t available in Scotland, the picture is similar and 15% fewer patients started treatment for lung cancer following an urgent referral for suspected cancer between April 2020-June 2021 compared with the same time period in 2019.
Download our one-page guide highlighting some of the key messages for health professionals, particularly GPs, on managing patients who are presenting with suspected lung cancer during the pandemic and reinforcing the importance of being alert to the risk of lung cancer in patients.
Download the recognition and referral of suspected lung cancer during COVID-19 guide
Urgent referrals for suspected urological cancers have been amongst the slowest to recover during the COVID-19 pandemic. In England, urgent referrals for suspected urological cancers were 25% lower between April 2020-March 2021 compared with the same time period in 2019-2020, which equates to around 55,700 fewer people [1]. While this data is just for England, we anticipate the picture is similar in Northern Ireland, Scotland and Wales. We continue to monitor the activity and you can find the most recent statistics on the COVID-19 stats page here.
We acknowledge there were various challenges in the recognition and referral of suspected urological cancers in primary care which existed before the pandemic. Spotting cancer is trickier when patients present with non-specific symptoms and/or co-morbidities. For example, symptoms of bladder cancer can often have alternative diagnostic explanations, such as urinary tract infections [2].
Additional challenges, exacerbated by the COVID-19 pandemic, include changes in patient behaviour, e.g. a reduction in people going to their GP with signs and symptoms of cancer [3], as well as accessibility challenges linked to remote consultations for certain groups, including older patients [4,5], and those with limited technical literacy [6] . There is also potentially less opportunity for point of care testing and physical examinations during remote consultations.
These additional challenges during the COVID-19 pandemic might be contributing to the reduction seen in the number routine referrals being made, which is of concern given the sizeable proportion of urological (in particular, prostate) cancer patients usually diagnosed via this route.
Key actions for Health Professionals for suspected urological cancer
| Be aware of the lower referral rate for urological cancers during the pandemic (and ongoing). | |
| Be aware and vigilant of patients at risk of urological cancer particularly older patients. | |
| Use national and local guidance to help guide decision making and make use of the low referral thresholds in line with NICE NG12 (England and Wales) and SRG (Scotland) where possible. | |
| Be aware of the potential challenges associated with remote consultations. | |
| Face to face appointments should be offered to patients presenting with urological symptoms. | |
| Take advantage of Advice and Guidance channels/platforms where available to inform decision-making and assessment of cancer risk prior to referral. | |
| Ensure robust safety netting processes when symptoms persist, worsen or change. | |
| Reassure patients that safety precautions regarding COVID-19 are in place in both primary and secondary care. |
Key actions for health professionals specifically for suspected bladder and kidney cancer
Reducing late stage, advanced prostate cancer will increase treatment options and improve outcomes. 100% of people will survive prostate cancer for 5 years or more if they are diagnosed at stage 1, compared with around half (49%) of people when diagnosed at stage 4 [7].
|
Key actions for health professionals specifically for suspected prostate cancer
Reducing late stage, advanced prostate cancer will increase treatment options and improve outcomes. 100% of people will survive prostate cancer for 5 years or more if they are diagnosed at stage 1, compared with around half (49%) of people when diagnosed at stage 4 [7]
|
Be aware of the low urological referral rate during the pandemic (and ongoing); likely driven by less suspected prostate referral. Around 10,200 fewer people were diagnosed with prostate cancer during April-December 2020 compared to the same months in 2019. [8] |
|
| Act on clinical suspicion with consideration of risk factors such as family history and black ethnicity. [2] | |
| Be aware of the potential challenges associated with remote consultation and suspected prostate cancer. | |
| We encourage you to conduct face to face appointments/testing with patients if there is suspicion. | |
| Take advantage of Advice and Guidance channels/platforms. |
‘Help us to Help You’ Campaign (England only)
NHS England launched a ‘Help us to Help You’ campaign which focused on the signs and symptoms which could indicate abdominal, urological cancers and lung cancer. The campaign targeted adults aged 50+ from lower socioeconomic groups and ethnic minority groups at higher risk of cancer. It was a multi-channel campaign with activity on TV, radio, social media platforms, digital and poster. Information was available in accessible formats (BSL, Braille, audio, large print and translated versions).
For more information on NHSE Help us to Help You Urological Campaign click here.
Education events supporting recognition and referral of suspected urological cancers
Gateway C hosted a Urological webinar on 27th October 2021. If you are registered with Gateway C you can watch the recording of the webinar. Click here(link is external) for more information
Urological cancer eLearning content
Access free CPD e-learning content to support you with the recognition and referral of suspected urological cancers on Doctors.net. Complete the module here or access a short message series here (login required).
Health professional perspective
Watch an updated video with Dr Joe Mays, Cancer Research UK GP discussing some of the key challenges and actions to consider when managing patients with suspected urological cancer in primary care.
Education events supporting recognition and referral of suspected urological cancers
Gateway C are hosting a Urological webinar on 27th October 2021. Registration opens soon. Click here for more information
References
[1] Data source: NHS England Monthly Provider-based Cancer Waiting Times.
[2] Carney M, Quiroga M et al. Effect of pre-existing conditions on bladder cancer stage at diagnosis: a cohort study using electronic primary care records in the UK. Br J Gen Pract 2020;70:e629-e635.
[3] Cancer Research UK commissioned medeConnect who surveyed 1003 regionally representative UK GPs online between 5th and 24th June and 1004 GPs between 4th and 30th September 2020. medeConnect is a division of Doctors.net.uk.
[4] McKinstry, B., Watson, P., Pinnock, H., Heaney, D. and Sheikh, A. (2009) Telephone consulting in primary care: a triangulated qualitative study of patients and providers. British Journal of General Practice, 59(563), pp. e209-e218.
[5] Mold F, Hendy J, Lai YL, de Lusignan S. Electronic Consultation in Primary Care Between Providers and Patients: Systematic Review. JMIR Med Inform. 2019;7(4):e13042. Published 2019 Dec 3. doi:10.2196/13042.
[6] Randhawa, R., Chandan, J., Thomas, T., & Singh, S. (2019). An exploration of the attitudes and views of general practitioners on the use of video consultations in a primary healthcare setting: A qualitative pilot study. Primary Health Care Research & Development, 20, E5. doi:10.1017/S1463423618000361.
[7] Office for National Statistics, Cancer survival by stage at diagnosis for England, 2019.
[8] Lloyd, T et al. Lifetime risk of being diagnosed with, or dying from, prostate cancer by major ethnic group in England 2008–2010. BMC Med 13, 171 (2015). https://doi.org/10.1186/s12916-015-0405-5.
The COVID-19 pandemic has had a significant impact on patient behaviour, with fewer patients seeking help for serious diseases than expected. There have been a number of national campaigns to encourage the public to contact their GP and NHS more generally. in England, Scotland, and Wales.
CRUK ran a short film on Digital TV and social media channels in June and again throughout September and October 2020 to support this. Patient presentation and urgent referrals continue to slowly recover, however referrals for some cancer types such as lung cancer have been more impacted and are further behind recovery compared to that seen in others.
Public Health England and the Scottish Government also ran public facing campaigns to raise awareness of lung cancer symptoms and to encourage people to seek help from their GP.
CRUK ran a multi-channel campaign in Wales during August and September 2021, which aimed to positively influence the public's attitudes to help seeking to ultimately encourage timely presentation to their GP for potential signs or symptoms of cancer. The campaign was a repeat of a campaign which ran in June and targeted adults aged 50+ from lower socio-economic groups in Wales. It ran for 6 weeks over TV, social media, on pharmacy bags and in newspaper adverts.
GPs in Wales were informed of the campaign prior to launch, through marketing channels including emails and promoted posts on Twitter to highlight that there may be an increase in presentations and they were provided with information on safety netting to support the management and onward referral of patients.
‘Help us to Help You’ Campaign (England only)
NHS England have delivered a number ‘Help us to Help You’ campaigns during 2020 and 2021 which focus on the signs and symptoms which could indicate abdominal, urological cancers and lung cancer. The campaigns targeted adults aged 50+ from lower socioeconomic groups and ethnic minority groups at higher risk of cancer. They have been multi-channel campaign with activity on TV, radio, social media platforms, digital and poster. Information was available in accessible formats (BSL, Braille, audio, large print and translated versions).
See links below for previous campaigns to encourage patients to seek help from their GP.
During COVID-19 around 3 million fewer people were screened via the bowel, breast or cervical cancer screening programmes in the UK than we would expect under normal circumstances* Cancer screening was effectively paused from late March 2020 across the UK nations, and restarted from ~June 2020
Screening programmes are now working through the backlog but due to the impact of COVID-19 on health services access continues to vary across each nation and programme.
As invitations are sent and follow up tests resume, there will be perceived risks as well as emotional and physical barriers to attending appointments for patients. Practice staff are in an ideal position to reassure patients of the safety measures in place for cervical screening as well as informing patients about participating in bowel and breast screening.
See the screening resource below for some useful tips for how your practice can support people to access cancer screening services.
*CRUK estimate based on weekly average number of people screened via bowel, breast and cervical screening programmes.
COVID-19 has reinforced the importance of safety netting. These unprecedented times have prompted rapid changes to pathways and shifts in patient and health professional behaviour, as well as creating a significant patient backlog. This has the potential to impact patients and undermine our efforts to see fewer people diagnosed with late stage cancer. During the recovery phase, robust safety netting protocols are important for mitigating the impact of COVID-19 on patients.
Our guide includes key safety netting tips, organised around some of the patient scenarios that the pandemic has brought to the fore.
Prior to COVID-19, there was variable use of the Faecal Immunochemical Test (FIT) in low risk patients who didn’t meet the criteria for urgent suspected cancer referral (NICE NG12 or Scottish Cancer Referral guidelines, where applicable) with pockets of FIT being used in other, including higher risk; patients prior to referral with lower GI symptoms.
The impact of COVID-19 on health services has meant local health systems have sought to manage demand and reduce unnecessary patient risk. The use of FIT in patients who meet criteria for urgent suspected cancer referral (‘high risk’) has been accelerated with a view to helping to prioritise the limited endoscopic capacity to those most in need.
For patient facing information see our COVID-19 and Patient Cancer Hub
For information on the impact of COVID-19 on cancer services see our CRUK COVID-19 and cancer blog
For information on the GP contract 21/22 for practices and PCNs see our GP Contract Hub
If you have any questions or feedback on the about this information please contact earlydiagnosis@cancer.org.uk