Our priorities for brain tumour research
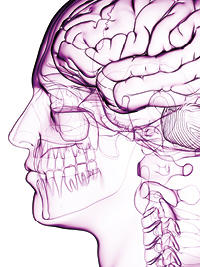 Brain tumour survival remains low, and has changed little in over a generation, which is why we made them a strategic priority as one of our cancers of unmet need. We've identified the top themes which we believe need to be addressed in order to transform the field.
Brain tumour survival remains low, and has changed little in over a generation, which is why we made them a strategic priority as one of our cancers of unmet need. We've identified the top themes which we believe need to be addressed in order to transform the field.
Progress in brain tumour research has been hindered by huge gaps in our knowledge, in particular of the biology underpinning the diseases. In 2016, we convened a panel of brain tumour experts from around the world to identify the questions in brain tumour research which, if answered, could remove these barriers to progress. While not an exhaustive list of all the challenges faced by those researching brain tumours, we believe that tackling these six themes will significantly accelerate progress for patients.
Our approach
We want to support the research that will make a real difference to people with brain tumours. To achieve our ambitions for brain tumour research, we are:
- Spending around £25 million over the next five years on ring-fenced, targeted initiatives
- Expanding our broad research portfolio across the discovery and translational research pipeline, and in all types of brain tumours, whether paediatric or adult, through our existing response-mode funding schemes
- Building a dynamic, multidisciplinary research community in the UK through training, recruitment and by helping people in other fields shift their focus to brain tumour research
- Developing the infrastructure required to facilitate innovation in the field, and create hubs of expertise
Our top priority research themes
![[Brain icon]](/sites/default/files/brain_-_200px_with_padding.png)
Leveraging neurobiology and neurodevelopment to unlock new mechanistic insights
This theme is about adapting and translating the wealth of neuroscience research (including, but not limited to cellular & molecular neuroscience, neurodevelopment, glial biology, and research focused on other diseases of the brain) to expand our knowledge of brain tumour initiation, maintenance and progression.
Understanding how brain tumours arise in both the developing and adult brain is likely to reveal important insights about brain tumor biology and may even identify new therapeutic opportunities. Many brain tumours, especially paediatric ones, are characterised by mutations in key developmental pathways, fueling the hypothesis that these tumours are developmental disorders. Understanding whether neural stem and progenitor cells are cells-of-origin in certain niches in the brain is also crucial, given that the cell-of-origin can dictate biological subtype and functional phenotype. There is also significant potential to explore links between brain tumours and other neurological disorders (such as those associated with demyelination or neurodegeneration). This theme gives teams the opportunity to coalesce around identifying how networks driving processes in the developing or diseased brain (such as differentiation, motility, patterning and proliferation) are co-opted by brain tumours.
![[Magnifying glass icon]](/sites/default/files/small_-_png-research_type_blue_rgb_screen_-_200px_with_padding.png)
Exploiting the brain tumour environment for clinical benefit
This theme is about deriving deep mechanistic understanding of tumour-environment cross-talk, to inform the development of innovative detection or treatment strategies.
Brain tumour behaviour is heavily influenced by the ecosystem around it. The brain tumour microenvironment is unique, comprising vasculature, cell types and an extracellular matrix which are unlike those found elsewhere in the body. In addition, the blood-brain barrier is a major obstacle for the delivery of systemic therapies to the brain. Its role in brain tumours is highly context-dependent and how its structural and functional integrity changes during disease progression remains largely unknown. Understanding the mechanisms that determine whether passage across the barrier is granted or not is crucial to improving delivery of therapies to the brain. A deeper understanding of the components of the brain environment, and how they interact with the tumour is likely to reveal new avenues for detection of clinical intervention. These insights are also likely to help boost the efficacy of immunotherapies, which have been largely disappointing against brain tumours thus far. In addition, brain tumour cells are reported to be highly invasive. Understanding the origins of these characteristics may provide useful angles for therapeutic intervention.

Developing better treatments that are based on brain tumour biology
This theme is about developing more effective treatments for brain tumours, based on solid biological rationale. The outputs of the research may include (but are not restricted to) small molecules, peptides, antibodies, nucleic acids, vaccines or radiotherapeutics).
Large-scale ‘-omics’ studies have helped classify some types of brain tumours into discrete molecular subsets, but these insights have been slow to translate into diagnostic or therapeutic opportunities. This theme invites teams to design innovative treatments that are based on the unique biology of the brain tumour and / or its environment. The therapeutic targets may include those that are identified from -omics studies as unique to brain tumours or that are commonly seen in other tumours but that have been difficult to drug. Teams should be able to demonstrate that target engagement would be both safe and clinically meaningful, and due consideration to blood-brain barrier penetration should also be given. Finally, we urge teams to take into account the significant tumour heterogeneity observed in brain tumours, and the myriad of resistance mechanisms that are likely to emerge.
![[Cell culture icon]](/sites/default/files/cell_-_option_2_blue_-_200px_with_padding.png)
Establishing pre-clinical models that accurately recapitulate disease trajectory or predict response to therapeutic challenge
This theme is about developing better models of brain tumours to increase confidence in the pre-clinical space, and accelerate the translation of promising agents into clinical trials.
The dearth of preclinical models that accurately recapitulate the human disease is one reason why so many novel agents fail in patients, despite having shown promise in the preclinical setting. Another issue is discord between the clinical context in which these studies are performed. Preclinical studies of novel agents are usually performed on treatment-naïve mice whereas clinical trials tend to take place in the relapsed setting, after patients have had a plethora of treatments, including those that drive tumour heterogeneity and thus increase the likelihood of resistance mechanisms. Here, a successful approach should draw on a deep understanding of neuroscience and target biology to develop innovative models (including but not limited to genetically engineered mouse models, patient-derived xenografts, organoids or microfluidic-based approaches), together with a thoughtful approach to validating and using them.
![[DNA icon]](/sites/default/files/small_-_png-broken_dna_-_200px_with_padding.png)
Using ‘-omics’ data to deliver precision medicine to brain tumour patients
This theme is about designing and validating a new multimodal taxonomy system for brain tumours, to facilitate the development of an integrated, interactive framework to deliver personalised care.
Current methods to diagnose both adult and paediatric brain tumours rely heavily on histopathology, which provides only limited information. Moreover, failure to fully incorporate the myriad of data gleaned by genomic, epigenetic, cell-of-origin, and transcriptomic studies means that information pertaining to molecular subtype or potential therapeutic vulnerabilities remains unleveraged. Although World Health Organisation diagnostic guidelines were recently updated, there are still several types of tumours whose diagnosis is based solely on histology. A more robust classification system would significantly facilitate the stratification of patients for biologically rich experimental medicine trials, helping match patients to treatments (both drugs and radiotherapy) that are most likely to work, and identifying the biological mechanisms behind treatment failure.

Identifying brain tumours that will respond well to gentler treatment
This theme is about identifying the biological features that distinguish tumours requiring aggressive treatment from those that do not.
Despite the wealth of ‘-omics’ data available for many different types of brain tumours, there are still significant gaps in our knowledge about the links between genotype and phenotype, and the molecular networks that correlate with particular clinical features remain unknown. In practice, this means that a ‘one-size-fits-all’ approach to treatment is usually adopted, raising the issue of whether some brain tumours would respond equally well to gentler treatment. This is a particularly pertinent issue in the paediatric space, where the long-term effects of treatment significantly affect quality of life. There is thus a real need to identify molecular signatures associated with clinical features such as recurrence. Developing a scientific framework that allows clinicians to maximise treatment efficacy, while mitigating the risk of long-term side effects is the essence of this theme.
Research opportunities in brain tumours
![[Brain icon]](https://main.stg.cruk.org/sites/default/files/styles/cruk_no_style/public/brain_-_200px_with_padding.png?itok=HhUZnLef)
Brain tumour survival remains low, and has changed little in over a generation. That's why we've made brain tumours a strategic priority as one of our four "cancers of unmet need".
We're boosting our investment into brain tumours, and we have a number of opportunities to help you develop your brain tumour research or to apply your skills to these cancers for the first time.

